AMD (Age-Related Macular Degeneration)
AMD - don't neglect your aging eyes...
WHAT IS AMD (MACULA DEGENERANCE)?
The macular region of the retina layer at the back of the eye provides a clear and detailed view of the objects. The term refers to a disorder in the visual center (macula) that develops with age. It is one of the leading causes of vision loss in those aged 65 years and over in the Western countries. Considering the increase in the elderly population, the importance of this disease increases.
WHAT IS AMD (MACULA DEGENERANCE)?
There are two types of macular degeneration that prevent the macula from performing its normal function.
Dry Type: 90% of macular degeneration is the dry type, yellow spots called drusen (formed by the accumulation of lipid-oily material under the retinal layers) are seen in the macula at the early stage. At this stage, the patient's vision is not severely affected. The progression of the dry type is usually very slow; however, vision loss is seen in very advanced stages. Multivitamin tablets may be useful in the treatment.
Wet Type: It is characterized by abnormal vascular structure under the macula or bleeding. It is formed by the progression of the defective capillaries occurred in the diseased area into the retina. Wet type can cause sudden vision loss. It is less than the dry type; however, it causes vision loss at 80%. Especially if the patient has membrane formation in one eye, the other eye is also in danger. (The disease starts in other eye within a year at the rate of 20%)
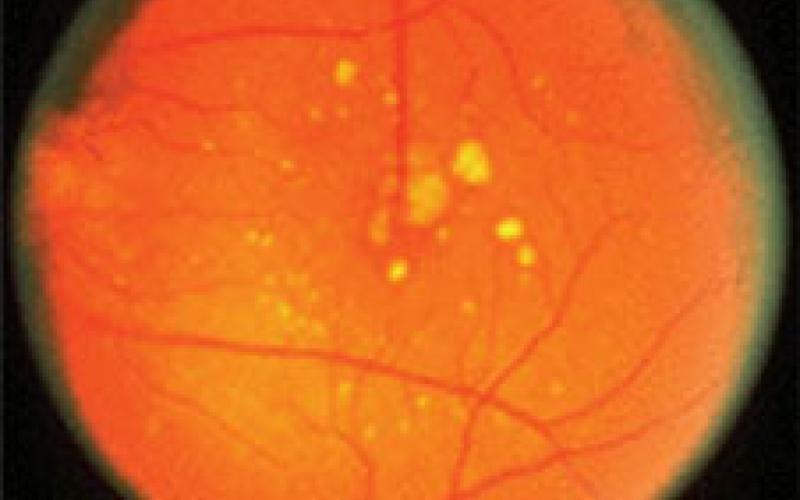
Dry Type
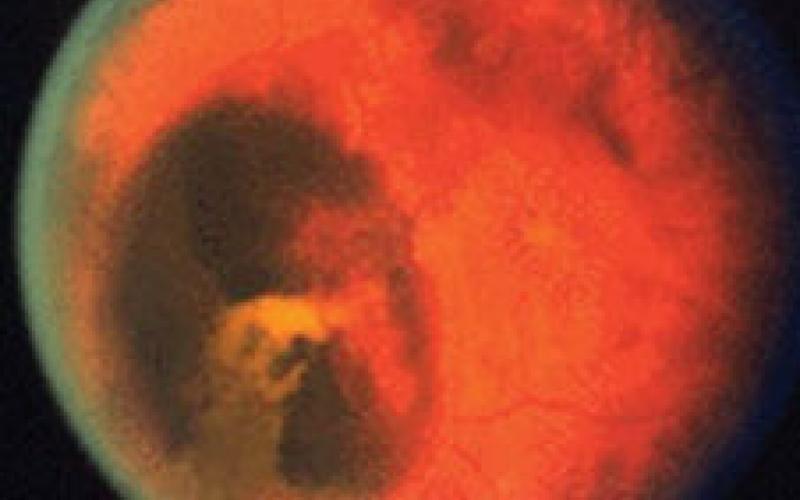
Wet Type
Both types are distinguished by eye ground examination and FFA (Fundus Fluoresceine Angiography). Patients may consult a doctor with complaints such as distorted vision, blurred vision, small vision, and seeing a dark spot in the area being examined. Sometimes the disease may not show any symptoms. In some patients, a rapid loss of vision may occur immediately after the onset of complaints.
WHAT ARE THE RISK FACTORS?
The real cause of macular degeneration is not well understood. Age seems to be the most important factor. As the quality of life increases and the average life expectancy increases, the incidence of the disease increases in the community. While the risk is 14% for 55–64 years, it is 20% for 65–75 years and 37% for 75 years. It is slightly more common in women than in men. Inheritance can play a role. It is scientifically proven that it is more common in smokers than in non-smokers. Some researchers suggest that high blood pressure, sunlight and high cholesterol are also risk factors.
WHAT ARE THE DIAGNOSIS AND EXAMINATION METHODS?
It occurs during optalmological examination by expanding the pupils with drops. Even small advances can be detected instantly with a so-called Amsler Card, which allows patients to test themselves even at home. The most important diagnostic aid is eye angioma. It is an examination of the presence of broken capillaries by taking photographs of the eye ground for 10 minutes following the administration of a medical dye from the arm veins. Depending on the dye used (fluorescein or indocyanin), there are two different techniques: FFA and ICG. If some patients are suspected of wet type and have an atypical appearance, two angiographies may need to be performed at the same time.
WHY IS EARLY DIAGNOSIS VERY IMPORTANT?
The earlier the diagnosis is made and the patient is followed up, the more loss of vision can be prevented. In the wet type, the smaller the membran is formed, the greater the chance of success is achieved. In the dry type, the patients are followed up and measures can be taken by making recommendations in terms of general health. Also, with the newly developed special drugs, at least the progression of the disease can be slowed down. Vitamins; some studies in recent years show that antioxidant vitamin and zinc intake slows down the course of the disease and reduces the risk of vision loss.
Argon Laser Therapy (ALT); laser treatment may be recommended especially for wet type macular degeneration, where the degeneration is away from the macular center. The membrane is destroyed by laser (photocoagulation) treatment. Retinal tissue that is treated with laser loses its ability to see; therefore, this treatment cannot be performed if the degeneration is located in the macular center. Laser treatment is performed to preserve existing vision and to stop the progression of the disease. It is not expected to regain the vision impaired.
Photodynamic Therapy (PDT); It is a new treatment method applied in wet type macular degeneration and it is becoming widespread worldwide. In addition to the known lasers, this new developing treatment method is a laser-sensitive drug (visudyne) of a certain wavelength, which is given through the arm veins. This drug is held only by the tissue formed by the abnormal vascular structure. After the drug is retained by this diseased tissue, a special laser is applied which affects only the area where this drug is held and does not harm the surrounding tissues and a special laser only used in this disease is applied. Thus, the formation of new vessels can be selectively eliminated and the capillaries can be closed without damaging the sensitive retinal layer of the eye. PDT inhibits the progression of the disease by 70%.
After PDT, patients should be protected from sunlight for 48 hours.

FFA Image
AUXILIARY METHODS FOR SLIGHT VISION
Unfortunately, there is no treatment for a large part of wet type macular degeneration and last stage dry type. There are a number of auxiliary methods to facilitate the lives of these patients who lose their central vision. There are very few auxiliary vision systems, ranging from a simple hand-held magnifier to sophisticated systems that magnify text and make it visible on the TV screen. Today, the most widely used system is telescopic glasses.
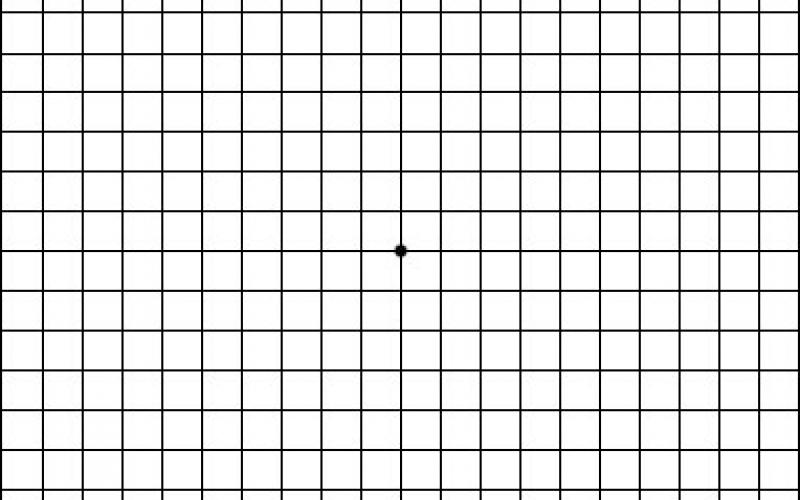
Amsler Grid Card
Look at the point in the middle of the figure with your other eye by closing one eye from your normal reading distance to this figure (and with your near glasses, if available). Then repeat the procedure with your other eye. If there are broken lines, distortions, faintness, dark areas, etc., consult your ophthalmologist immediately. Although this test is used to diagnose Macular Degeneration, the actual diagnosis can only be made by a detailed optalmological examination.

