Cornea and Diseases
WHAT IS CORNEA?
The cornea is a transparent glass-like layer covering the front of the colored part of the eye.

WHAT IS THE FUNCTION OF CORNEA?
The cornea is smooth and transparent like a glass; however, it is strong and durable, which helps the eye in two ways:
- Like a shield, it protects the inner parts of the eye against germs, dust and harmful substances. It shares this task with the eyelids, eye socket, tears and sclera (white part of the eye).
- It is the entrance of rays to the eye like a window and contributes 65-75% of the total refractivity of the eye. It also filters some of the UV rays.
WHAT ARE THE DISEASES AFFECTING CORNEA?
Allergies:
In particular, allergies related to pollen occur in dry and hot weather. Symptoms include redness, itching, tearing, burning, stinging and watering. The use of various cosmetic agents, medicines and contact lenses increases the incidence of allergy.
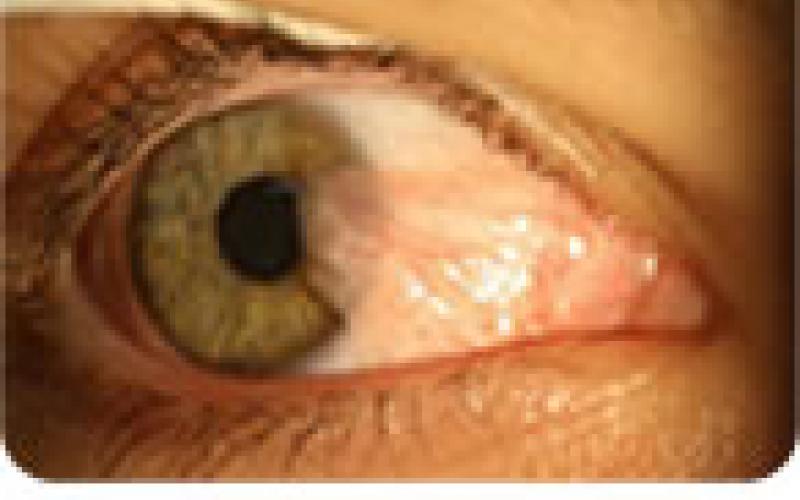
Conjunctivitis:
The conjunctiva is the tissue that covers the white part of the eye (sclera) and the lids. Infections cause swelling, itching, flushing and burning of the conjunctiva. Some types of conjunctivitis can easily be transmitted from person to person. Long-term conjunctivitis may cause inflammation and loss of vision in the cornea.

Corneal Infections:
Corneal damage can occur after infection of bacteria, viruses or fungi in various forms. Painful infections called keratitis may cause blurred vision, watering, burring and pain symptoms and whitening and spotting in the cornea.
Corneal Dystrophies:
Blurring of one or more parts of the eye with loss of normal transparency can often develop due to familial causes and sometimes unknown causes. It usually affects vision, while some may be detected in routine optalmological examinations.
Pterygium:It is the walking of pink colored triangular tissue onto the cornea. It is seen in people between 20-40 years in sunny environments. Surgical removal is not recommended unless it affects vision. It has a recurrent feature.
Corneal Ulcer:
When the eye remains open, dryness of the cornea and infection may occur, which causes corneal ulcer (ulcus cornea). Even visual loss may be encountered in later stages. For people at risk, the eye space can be narrowed by surgical method.
Dry Eye:
Continuous production and drainage of tears is very important for eye health. The tear provides nutrition to the cornea, heals wounds and protects the eye against infections. Tear production is low in patients with dry eyes. It is not possible to keep the corneal surface wet and comfortable. The most common symptom is stinging, such as sand, or foreign body sensation in the eye. It is more common in women especially after menopause. It can be seen in dry weather and during the use of various drugs and connective tissue diseases (rheumatoid arthritis, sjogren's syndrome, etc.)

Keratoconus:
It is the progressive thinning of the cornea and its cone shape by losing its normal curve and extending to the front more than normal. It changes the refractive power of the cornea and causes moderate and severe astigmatism and blurred vision.

Normal Eye

Eye with Keratoconus
HOW IS KERATOCONUS DISEASE TREATED?
|
Intacs Treatment: Intacs operation is performed for keratoconus patients and for the treatment of corneal complications occurring after failed or incorrect laser surgery. The corneal rings used are made of synthetic material and are round rings placed inside and close to the outer edge of the cornea. With the special surgical set of the Intacs device used in this operation, firtst the channels where the rings are placed are created. The rings are then inserted into the cornea. The rings are designed to form a 150 degree circle when placed. The rings press the circumference of the cornea and act by flattening this area. |
 |
Corneal Cross Linking (CCL) Treatment:
As we age, corneal collagen thickens and hardens. This is why there is no improvement in keratoconus findings in healthy individuals after the age of 40s. A similar situation is seen in diabetes (Diabetes Mellitus). Therefore, keratoconus findings do not progress in young patients with diabetes. The idea of Corneal Cross Linking treatment was born here. If the resistance of the corneal collagen is increased, the endurance of the cornea is increased and the progression of the keratoconus can be stopped. By using ultraviolet A and riboflavin in drop form, the bonds between the corneal collagen fibers are increased and the cornea becomes more resistant. Studies have shown that the progression of the disease is stopped and the corneal curvature is improved by 2 degrees on average. The aim of this treatment is to stop the progressive keratoconus disease, to reduce the refractive error, to improve visual quality and to eliminate the need for corneal transplantation (Keratoplasty). No harmful side effects have been observed in the studies.
Corneal Transplantation (Keratoplasty):
Corneal transplantation is the replacement of the a diseased or scarred cornea with the new one. In surgery, the blurred cornea at the central cornea is replaced with a transparent donor cornea from the eye bank. Corneal transplantation is a preferred treatment at the last stage because corneal donations are inadequate and expensive at the same time and the body is likely to reject the tissue by 15-20%.
WHAT ARE THE REQUIRED CONDITIONS FOR CORNEA TRANSPLANTATION?
Normally transparent and non-vascular corneal tissue may become blurred by the formation of wound tissue or edema (swelling). Turbidity of the cornea causes the light to be refracted properly and consequently reduces vision. Furthermore,
- In some genetically transmitted corneal diseases - as a result of damage to cells that keep the cornea transparent after eye surgery
- In case of wound tissue and new vascularization in the cornea due to infection (after Herpes keratitis)
- Impairment in natural dome- shaped cornea and keratokonus.
- If the cornea becomes blurred or severely impaired due to accidents
- If the body rejects the cornea after corneal transplantation, corneal transplantation can be performed.
In some cases, there may be severe pain as well as visual impairment. Corneal transplantation can be performed to improve vision, reduce pain or preserve eye integrity.
KORNEA NAKLİ AMELİYATI NASIL YAPILIR?
Generally, local anesthesia is performed by anaesthetizing the eye and its surroundings. However, general anesthesia can be performed in children, patients who cannot continue with local anesthesia or according to physician's preference. Under a microscope, a window with a diameter of 7.5–8 mm is removed from the center of the patient's blurred cornea with a special round knife and the healthy cornea is cut to the appropriate size and sutured to this area.
DOES THE CORNEA TRANSPORT OPERATION HAVE RISKS?
There is no risk-free surgery. Infection, bleeding, retinal tear (retinal detachment), eye pressure (glaucoma), loss of transparency of the lens (cataract formation) may occur among the complications (undesirable results). In addition, the patient's eye may reject the newly transplanted cornea and the cornea may become blurred. Besides, complications related to local or general anesthesia may develop.
HOW DOES TISSUE REJECTION OCCUR?
Tissue rejection is that the body's immune system recognizes the transplanted tissue and tries to get rid of it. It shows signs of blurring and vascularization in new corneal tissue. Because the cornea is vein-free, it is very advantageous over all other organs and tissue transplants, and tissue rejection is rare. Tissue rejection occurs more frequently in the cornea of the transplanted person, if there is already extensive vascularity. In addition, loosening or rupture of the sutures, inflammatory conditions in the eye, eye pressure, adherence of iris tissue to the cornea increase the possibility of tissue rejection.
HOW TO UNDERSTAND TISSUE REJECTION?
In case of intense redness of the eye, sensitivity to light, decreased vision and pain in a transplanted patient, tissue rejection may be considered and an ophthalmologist should be consulted immediately.
CAN TISSUE REJECTION BE TREATED?
Tissue rejection is eliminated by treatment with cortisone (steroid) drops in most patients (90%). Cortisone drops suppress the recipient's immune system and prevent it from rejecting new tissue. In cases where the drops are not sufficient, it may be necessary to administer high doses of cortisone drugs intravenously. If the cornea becomes blurred again due to tissue rejection, the same eye can be transplanted again.

