Keratoconus and Treatment
Treatment method for patients with KERATOCONUS: CCL (Corneal Cross Linking)
WHAT IS KERATOCONUS DISEASE?
Keratoconus can be defined as the progressive thinning of the transparent refractive layer, called the cornea, which is like the hour glass in front of the eye, and extends in a forward conical manner. It is more common in women. It changes the refractive power of the cornea and causes moderate or severe irregular astigmatism and blurred vision. Swelling and whitening of the cornea may occur in the last stage of keratoconus disease.
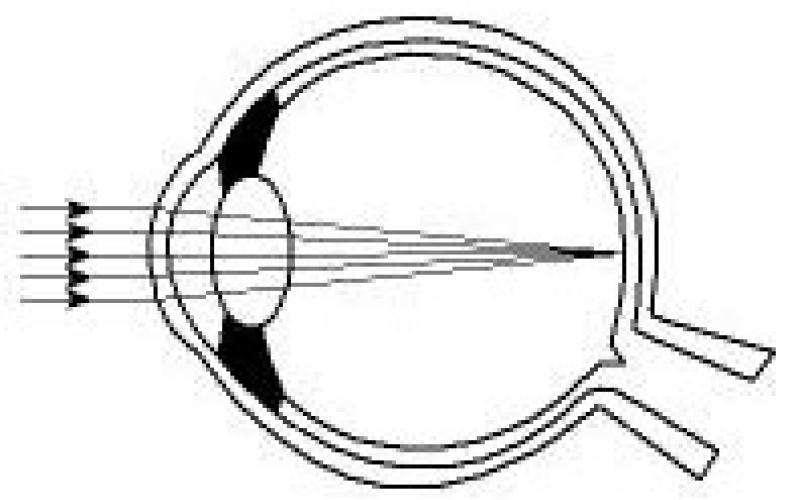
Normal Cornea and Refraction of Light
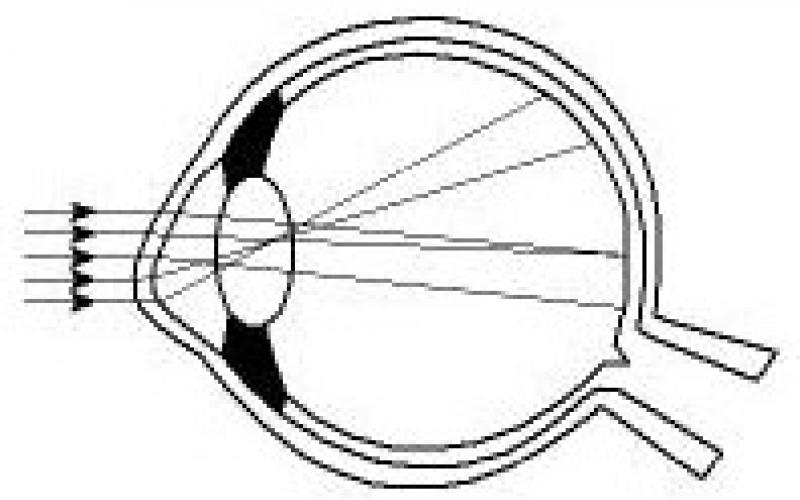
Cornea with Keratoconus and Refraction of Light
WHO HAS THE KERATOCONUS? WHAT ARE THE SYMPTOMS?
The disease has genetic transition and is seen in the relatives of keratoconus patients as high astigmatism or high keratoconus. Patients have increasing irregular astigmatism and myopia, and bilateral involvement occurs. The biggest complaint of the patients is the frequent change of glasses but shortly thereafter, the deficiency of these glasses and visual impairment. Keratoconus may be associated with corneal injury, some special eye diseases and systemic disorders. It may also occur in cases where the transparent layer of the eye is weakened after Excimer Laser surgery is performed on unsuitable eyes.
WHAT ARE THE RISK FACTORS?
Treatment of this disease, occurring every 2,000 people, should be started early. Especially people having relatives with such disorder should be more sensitive. Therefore, it is of prime importance in the diagnosis of the disease that parents take their children to an ophthalmologist and ensure that they are examined carefully and in detail. Allergic eye problems in people with anterior keratoconus symptoms cause rapid progression of the disease due to continuous scratching and rubbing. For this reason, examination is important in people with frequent eye allergy problems.
HOW IS DISEASE DIAGNOSED?
The symptoms of the disease usually occurring in adolescence is difficult to diagnose at childhood and can be determined by very detailed examinations. Many patients think they have only "myopic astigmatism". It develops between the ages of 20 and 40 years. In this period, eyeglass numbers start to change frequently and eye specialist can give prescription glasses with different numbers. The patient might not see clearly in spite of the glasses.
IS EARLY DIAGNOSIS VERY IMPORTANT?
This disease that is difficult to diagnose may result in blindness if not stopped. Nowadays, keratoconus patients can be diagnosed by chance during topographic examination for corneal examination especially in patients who do not want to use glasses and are considering Excimer Laser treatment.
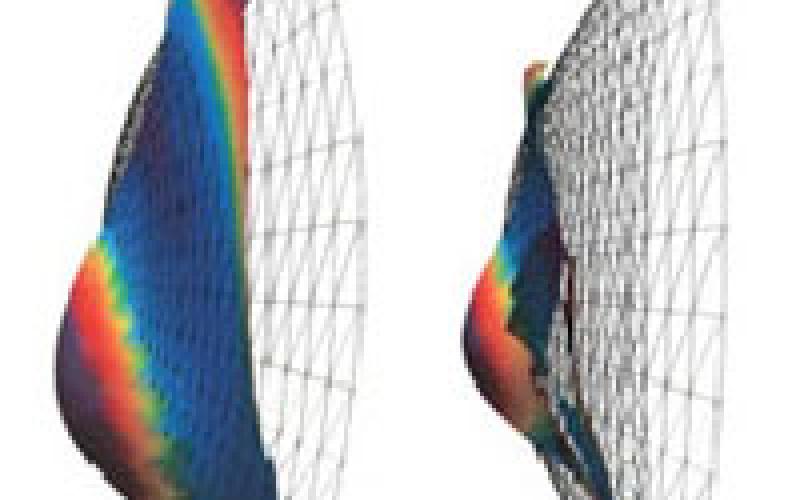
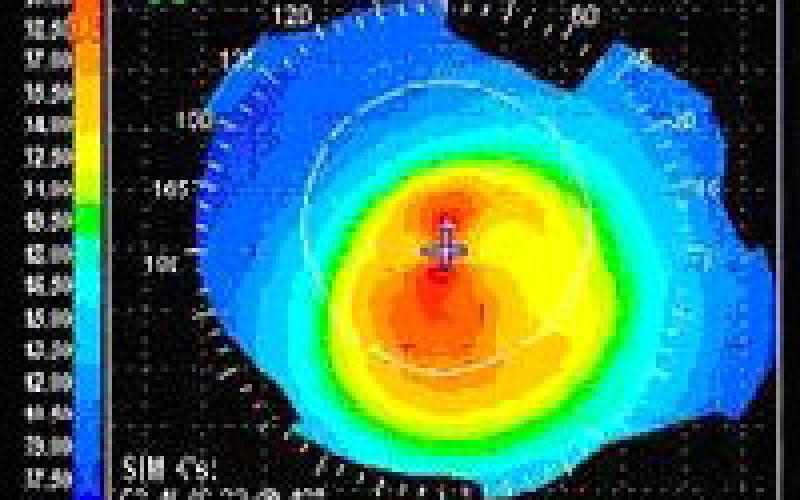
Corneal Topography of the Patient with Keratoconus
WHAT ARE THE TREATMENT METHODS?

Special solid contact lenses are used in the early stages of the disease. However, contact lenses cannot stop the progression of the disease. These lenses correct the curved area of the corneal center, hence the astigmatism, and improve vision by providing clear vision. However, as the disease progresses, they become insufficient and the vision gradually decreases. Another alternative treatment called Intra Corneal Ring (INTACS) is to insert a ring into the corneal layer. It may partially prevent the progression. Another alternative treatment is corneal transplant surgery. Corneal transplantation is a preferred treatment at the last stage because corneal donations are inadequate and expensive at the same time and the body is likely to reject the tissue by 15-20%. However, the application of Corneal Cross Linking considered to have been effective in recent years can prevent the progression of the disease.
WHAT IS CORNEAL CROSS LINKING (CCL) TREATMENT?
As we age, corneal collagen thickens and hardens. This is why there is no improvement in keratoconus findings in healthy individuals after the age of 40s. A similar situation is seen in diabetic patient (Diabetes Mellitus). Therefore, keratoconus findings do not progress in young patients with diabetes. The idea of Corneal Cross Linking treatment was born here. If the resistance of the corneal collagen is increased, the endurance of the cornea is increased and the progression of the keratoconus can be stopped. By using ultraviolet A and riboflavin in drop form, the bonds between the corneal collagen fibers are increased and the cornea becomes more resistant. The aim of this treatment is to stop the progressive keratoconus disease, to reduce the refractive error, to improve visual quality and to eliminate the need for corneal transplantation (Keratoplasty).
Pre-treatment checks and examinations:
- Vision level with and without glasses
- Refraction defect with and without drop
- Corneal topography (map of the anterior surface of the cornea)
- Corneal thickness
- Endothelial cell count
- Fundus (eye ground) examination
HOW IS CCL TREATMENT APPLIED?
In order to apply this treatment, it is important to determine the fact that the disease is progressive. As a result of detailed examinations, it is revealed that the disease is progressive and then treatment is applied to the appropriate patients.
Dropping Riboflavin (Vitamin B2):
- The eye is anesthetized with topical anesthetic drops before the procedure.
- Following topical anesthetic drops, the corneal epithelium is mechanically removed with a blunt spatula.
- Riboflavin solution is dropped to the cornea with epithelium removed for 30 minutes with 2 drops at 5 minutes internals.
Application of UV Light:
- After 30 minutes, the patient is placed on a biomicroscope.
- After riboflavin fluorescence is seen in the anterior chamber, 370 nm UV is applied for 30 minutes in an area of approximately 7 mm at a distance of 4-5 cm from the corneal surface.
- During the UV application, 2 drops of Riboflavin are dropped every 5 minutes.
- After the procedure, bandage is applied to the eye and the eye is not closed.
Since the corneal epithelium is self-renewing, the epithelium scraped during the operation is completely healed after approximately 3 days. During this period, patients may experience some pain, stinging and burning sensation. After the treatment, the drops are used for 1 month.
WHAT IS THE SUCCESS OF CCL TREATMENT?
We can find out whether or not the treatment is successful within 3 months. Visual quality and visual acuity increase in patients with keratoconus especially at the beginning and middle stage; the disease progression stops.

